Introduction
Lateral dislocation of the patella with rotation around its vertical axis, otherwise known as vertical patellar dislocation (VPD), is a significant injury that results in the patella’s articular surface facing medially or laterally.1 Most lateral patellar dislocations occur as a result of a rotational injury and approximately 10% of patellar dislocations occur due to a blow to the medial aspect of the knee.2,3 In general, the reported mechanisms of VPD consist of a direct blow to the knee during sports, a twisting injury, or significant traumatic force.1,4–7 VPD is an incredibly rare injury and, as of recently, only 30 case reports exist in the current literature.1 While many of these reports describe this injury in adolescent boys, according to Udogwu and Sabatini,1 in addition to their case report, only 4 others have detailed this injury in a pediatric female patient. We report a rare case of irreducible lateral dislocation of the patella with vertical axis rotation following a simple fall from standing in an adolescent girl with a history of significant developmental delay requiring open reduction and medial repair.
Case Report
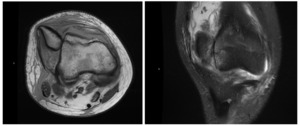
A 13-year-old adolescent girl, with a history of developmental delay and left knee patellar instability, presented to the emergency department 4 days after an injury to the right knee. The patient reported a fall from standing directly onto the anteromedial aspect of the right knee on a carpeted floor, resulting in immediate pain and swelling. Per the patient and her family, this was her first reported lifetime patellar dislocation of her right knee. At the time of presentation to the emergency department, the patient reported no pain with sitting, but significant pain with weight bearing and reduced range of motion of the right knee. Radiographs demonstrated a laterally dislocated patella (Figure 1). After several failed attempts at closed reduction, the patient was placed in a knee immobilizer and was urgently referred to the orthopedic clinic. For unknown circumstances, the patient did not present to our clinic until 10 days after sustaining the injury to her right knee. Magnetic resonance imaging was obtained, which was significant for a fixed lateral dislocation and rotation about the vertical axis of the right patella (Figure 2). The magnetic resonance imaging also showed attenuated medial patellofemoral ligament (MPFL) with high-grade/complete tearing towards the patellar attachment. On physical examination, the patient had pain with 90 degrees of flexion, crepitus with both flexion and extension, and a visible gross deformity at the lateral aspect of the knee. No numbness, tingling, or loss of sensation was noted. Discussion was had with the family regarding the need to proceed with surgical intervention and a plan was made for general anesthesia and open reduction of the fixed patellar dislocation with medial repair vs reconstruction. In general, MPFL reconstruction requires additional surgery including suture anchors and interference screws to be placed in the bone as well as a graft from either the patient or a donor. There is also additional time following these procedures for recovery. In this case, given this patient’s significant developmental delay, the family wished to move forward with medial repair because this was a more simple and straightforward surgery.
One day after presentation to the clinic, she was taken to the operating room. Under general anesthesia, another attempt at closed reduction was unsuccessful. The decision was then made to proceed with open reduction, which was then performed through a medial parapatellar incision. Inspection of the quadriceps and patellar tendon revealed vertical axis twisting and fixed lateral dislocation of the patella. The patella was reduced with gentle sweeping motion of the finger. When range of motion (ROM) was tested, the patella was unstable when moving past 60 degrees of flexion. The knee joint was inspected, with no sign of intra-articular loose bodies. Medial and lateral femoral condyles had no evidence of osteochondral fracture or cartilage fissuring. A partial-thickness fissuring of the medial patellar facet was visualized without loose osteochondral fracture. A medial retinacular repair and imbrication was completed. Knee ROM was retested and was stable from 0 to 90 degrees. Anatomic reduction of the patella was confirmed with biplanar fluoroscopy. The wound was then irrigated and closed in layered fashion. After the operation, the patient was instructed to weight bear as tolerated with the use of a brace locking the knee in full extension. Physical therapy was prescribed to progress ROM by 20-degree increments each week. Postoperative management throughout the entire course of recovery was uneventful. An x-ray at 2-week follow-up demonstrated excellent reduction and alignment (Figure 3). Three-month postsurgical follow-up demonstrated no sign of knee instability, full ROM, and mild discomfort after physical therapy. The patient was then discharged from outpatient care. She was instructed to continue use of the knee brace and physical therapy, and return to clinic if needed.
Discussion
A number of case reports have detailed lateral patella dislocation with vertical axis rotation in pediatric patients; however, many of these reports involved significant trauma or a rotational force causing the injury.1,4–7 Interestingly, Devgan et al8 reported the case of a 14-year-old adolescent boy who experienced this injury while running on uneven ground. Notably, this patient did not report any trauma or rotational force.8 We are unaware of any cases reported that describe such a significant injury following a minor nontraumatic incident as detailed in this report. Adding to the unique characteristics of this case are the patient’s history of significant developmental delay and the positive outcome as a result of open reduction and medial repair without the need for MPFL reconstruction.
This case highlights a rare injury seen in pediatric patients. We recognize the unfortunate reality that this patient did not present to our clinic for a period of 10 days following her injury. However, the delay in presentation to the clinic, following initial admission to the emergency department, did not impact the decision to pursue open reduction and medial repair. As noted in the literature, closed reduction of a laterally dislocated patella with vertical axis rotation is difficult to accomplish and repeated attempts may cause osteochondral damage.4,8 We recommend the use of open reduction in most of these cases in order to avoid further injury. Once reduction is obtained, the decision must be made to proceed with medial repair vs MPFL reconstruction. Generally speaking, the literature suggests that MPFL reconstruction has better outcomes than medial repair in cases of patellar instability.9 However, no such studies exist comparing these interventions in cases of VPD. In this patient with a first lifetime dislocation of this knee, history of developmental delay, and open distal femoral physis, after discussion with the family who wished to pursue the simplest intervention possible, the decision was made to perform a medial repair and plan for reconstruction if additional instability events were to occur. MPFL reconstruction should be considered in patients with recurrent instability events and those with increased risk for future instability.
Statement of informed consent
Patient and parents have been informed that the data concerning the case would be submitted for publication and have consented.